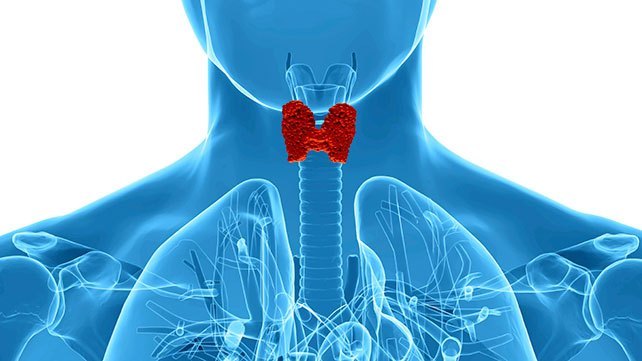
This month I focused on thyroid health awareness with my corporate clients. Considering it affects over 20 million men and women in the US and growing in numbers, it’s hard to keep up with all the continuous information out there. Women are 5-8 times more likely to develop a thyroid issue than men and sometimes, the 1 out of 8 women that do develop thyroid disease have it for years before they are diagnosed. It’s possible to reverse, but it can be a lengthy process with so many unwanted symptoms given; fatigue, brain fog, weight-gain, mood swings and brittle hair and nails, just to name a few. This affects men, too and can actually be overlooked for men, since physicians link thyroid issues to peri-menopause and post-pregnancy.
One important piece that tends to go to the wayside is: what are the best thyroid markers to test and what are the optimal ranges? So many underlying conditions can affect your thyroid such as diet, underlying chronic illness (ex: diabetes) and infection (Lyme disease, SIBO), lifestyle factors (excess caffeine and alcohol), stress and post-traumatic stress, but how do we know where you’re body is at and what to exactly work on? Sadly, conventional medicine only test for two basic markers at best, your TSH and T4 hormones, but these are really only a small piece of the puzzle when it comes to getting you back to optimal thyroid function. As well, if these numbers fall within ‘normal’ range, we are told that there isn’t much to worry about, when in fact optimal ranges are key to feeling well and can have a significant impact on how you feel even when you fall within ‘low-normal or ‘high-normal’ range. Know that if your numbers are showing up as ‘normal’ and you’re still not feeling great, here is a better way to get a clearer explanation.
Let’s take a quick look at what is usually tested:
TSH (Thyroid-Stimulating Hormone): The hormone released by your pituitary to stimulate your thyroid to produce thyroid hormones.
T4: The storage form of your thyroid hormone.
Your TSH is a crucial source of information as to how your thyroid is working even though it is produced by your pituitary gland. If TSH levels are too high, contrary to what people may think, means that you thyroid is low and needs extra stimulation (hypothyroidism). If TSH levels are too low, this can indicate your thyroid is overactive (hyperthyroidism). This in conjunction with T4 is the primary thyroid hormone that stores the hormone and circulates throughout your bloodstream and into your tissues; however, the active thyroid hormone is T3. T4 converts into T3. So, guess what? If your body is functioning correctly, anytime T3 needs an extra push, it should be able to signal T4 to send that extra push. Think of T4 as your savings account and T3 signaling to send a little cash in your hand, but you’re never getting more or less than what you need. With that said, your T4 keeps your cash safely for when T3 needs it again.
But it doesn’t stop there! Here are the additional thyroid hormones you want tested for the full picture:
T3: the active form of thyroid hormone.
Free T4: the storage form of thyroid left free rather than bound.
Free T3: the active form of thyroid left free rather than bound.
TBG (thryoxine-binding globulin): the protein that binds to your thyroid hormone so that the hormone can move through your blood stream.
Reverse T3: a type of thyroid hormone that prevents free T3 from attaching to your cells, slowing down the active form of T3, important when diagnosing autoimmune thyroiditis Hashimoto’s (a form of hypothyroid).
The thyroid is compromised of such a delicate system depending on our HPT–axis (hypothalamus-pituitary-thyroid axis), HPA-axis (hypothalamus-pituitary-adrenal axis), in conjunction with our stress hormone, cortisol, that all of these factors put together are the reason so many doctors and practitioners can miss important information. For instance, if your TSH and T4 show an optimal range but your Reverse T3 is high, you’re likely converting too much T4 to RT3, another inactive form of thyroid hormone, which can cause hypothyroid symptoms. This is why so many of us are told things are fine, when behind the scenes things may not be so fine!
Thyroid antibodies (TPOAb) and thyroglobulin antibody (TgAb): biochemicals produced by your immune system to attack your thyroid.
If your antibodies are elevated, this can indicate that your immune system is attacking your thyroid and you have an autoimmune thyroid disease or on the spectrum for an autoimmune disorder.
Today, the conventional range for TSH is 0.5 – 5.0 uIU/mL; a super wide range. Once narrowed by the American Association of Clinical Endocrinologists in 2003 to 0.3 – 3.0 uIU/mL, conventional physicians still use the wider range. Not sure why! A 3.0 is considered pretty high, a 5.0 is way out there. Here is a guideline to see optimal ranges for yourself or loved ones, regardless of what range is used:
TSH 1.0 – 2.0 uIU/mL or lower (Levothyroxine or Armour can artificially suppress TSH. Pregnant women <2.5 uIU/mL.
FT4 >1.1ng/dL
FT3 >3.2pg/mL
RT3 <than a 10:1 ratio of RT3 to FT3
Thyroid peroxidase antibodies <9IU/mL or negative
Thyroglobulin antibodies <4IU/mL or negative
It’s also important to truly listen to your body and communicate symptoms that may not match up with lab results. When I’m working with clients, blood work doesn’t tell the full story. Knowing your body, communicating your symptoms and having a practitioner that can order the correct panels and probe for underlying issues is what really hashes out the ever so multi-faceted thyroid issue. You do deserve to have a health advocate dig deeper than the numbers and to find the root cause of what is making you feel the way you do. Don’t let anyone tell you differently!
In fact, next up I’ll be talking about what nutrient deficiencies can affect your thyroid health and how to go about incorporating them through diet and proper supplementation. Stay tuned…
References:
- J. Garber, R. Cobin, H. Gharib. AACE Journal. Clinical Practice Guidelines for Hypothyroidism in Adults. 2012. https://journals.aace.com/doi/abs/10.4158/EP12280.GL
- K. Lewandowski. Thryoid Research. Reference ranges for TSH and thyroid hormones. 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4480274/
- O. Koulouri, MRCP, C. Moran, MRCPI, D. Halsall, PhD, FRCPath. Pitfalls in the measurement and interpretation of thyroid function tests. Best Practice & Research, Clinical Endocrinology & Metabolism. 2013.